Osteoporosis – How you can have stronger bones
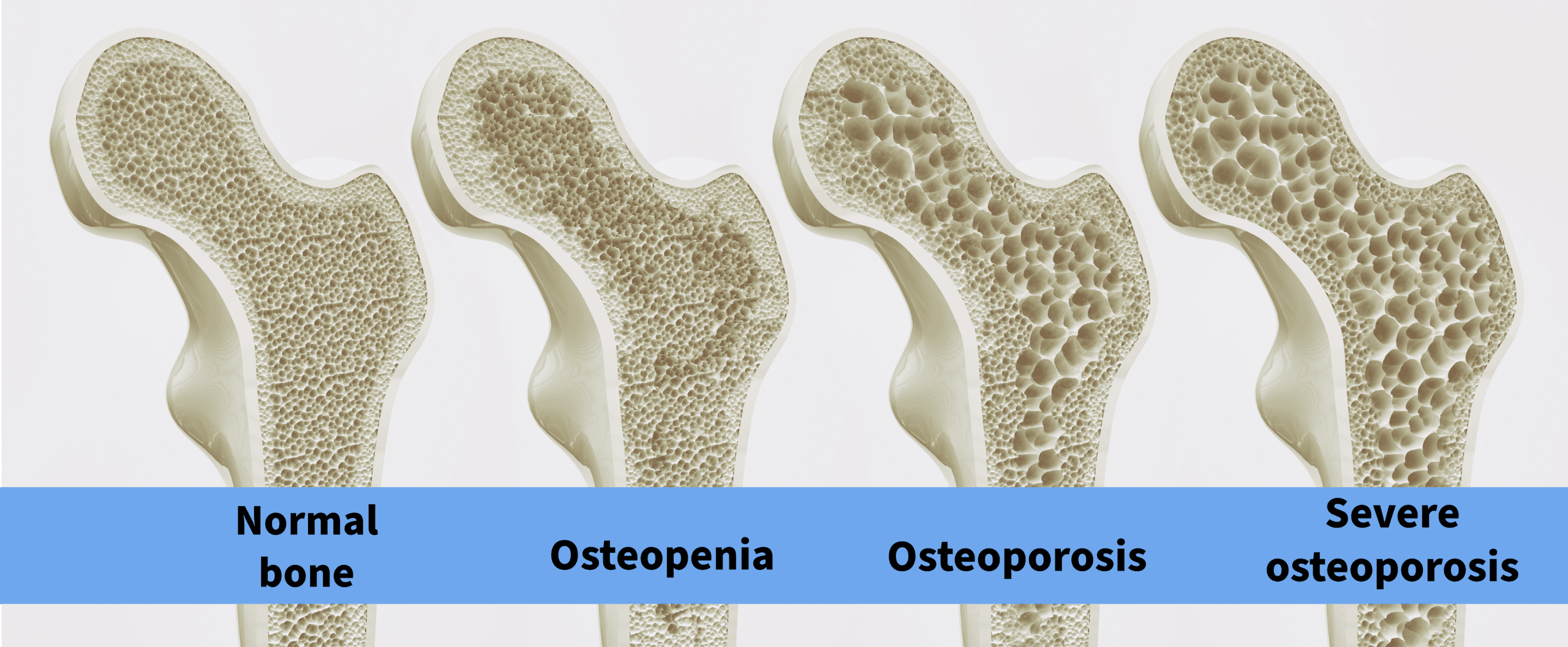
Osteoporosis is a silent disease. You can have significant bone loss with no signs or symptoms at all. Your bones need to last your entire life. Having strong bones will help you have a longer and better quality life.
Causes of Osteoporosis
- Deficiencies of vitamin D and vitamin K.
- Elevated levels of parathyroid hormone, commonly caused by longstanding unrecognized vitamin D deficiency.
- Mineral deficiencies – calcium, magnesium, boron, strontium, manganese, zinc, copper & silicon. Low intake of vitamin C and/or protein which weakens the collagen in bones.
- Low levels of the sex hormones estrogen, progesterone and testosterone, especially in premature menopause
- Medications such as long-term corticosteroids, antacid medications etc
- Gluten intolerance (often undiagnosed)
Vitamin D and Vitamin K
Take enough supplements of vitamin D3 and/or get enough sunshine to keep your vitamin D blood levels around 150 to 200 nmol/L. Calcium needs to be spread throughout the bones in the correct places and this is done by vitamin K.
Vitamin K 2 sources: natto, beef and lamb liver, oily fish, moldy cheese, egg yolks
Vitamin K1 sources: leafy green vegetables – good gut bugs convert K1 into K2. People with poor gut health lack these beneficial microbes.
TIP: Vitamin K and Vitamin D can prevent vertigo and dizziness.
Consume protein-rich foods for strong bones.
You need to consume one gram of pure protein per kilogram of your body weight daily. Good sources are meat, seafood, poultry, eggs, and yogurt and cheese. Bone broth provides your body with the building blocks for protein synthesis, including collagen.
Your bones need plenty of good quality protein to be strong.
Synd X protein Powder, glutamine and Muscle Food Powder can support muscle metabolism.
Nutrients for bone and collagen
Collagen Building.
Vitamin C, zinc, biotin, silica, and sulphur are required for collagen production.
Your bones are made of 40 percent hard collagen, which is a type of protein.
Collagen Food Powder contains all these things and can be added to drinks or water.
Calcium
A calcium supplement that contains a well absorbed form of calcium known as calcium citrate and calcium hydroxyapatite, plus the other bone essential minerals magnesium, manganese, zinc, silica, boron, and copper.
Avoid calcium carbonate supplements as they are poorly integrated into bone and can accumulate in arterial walls.
Other measures
Talk to your doctor about the use of treatments to prevent bone loss. You may need to see an endocrinologist who specializes in treatment of osteoporosis. Avoid falls by looking where you walk and never rush. Carry a small torch in your bag or pocket at night to see where you are going. Many people with osteoporosis never have any problems until they fall over and fracture a bone.
The Bioidentical Sex Hormones Testosterone, Oestrogen, and Progesterone can be used to preserve bone density in women with a Premature Menopause (under age 40).
Medications
Conventional treatment for osteoporosis is oral or intravenous Bisphosphonate drugs which stop bone turnover. Possible side effects include reflux and oesophagus inflammation. Rarely necrosis (death) of the jaw bone can occur.
Oral and intravenous bisphosphonates:
Alendronate (Fosamax®).
Risedronate (Actonel®).
Ibandronate (Boniva®).
Pamidronate (Aredia®).
Zoledronic acid (Reclast®, Zometa®).
Generally speaking Bisphosphonates drugs are recommended to be used for 5 years.
Denosumab (Prolia) Injections are effective in stopping bone loss and are injected every 6 months. Prolia can have side effects including an increased risk of infections, skin problems and aches and pains. If you stop using it suddenly, this may increase your risk for more bone fractures, which do not heal well. If you are having dental procedures, you may have an increased risk of jaw problems. To put it bluntly your jawbone may die!
Blood and Urine Tests for Osteoporosis
- C-terminal telopeptide of type 1 collagen (CTx)
- Crosslaps as a marker for bone resorption
- P1NP (Procollagen type 1 N-terminal propeptide)
- Bone-specific alkaline phosphatase (BALP) – People with osteoporosis generally have BALP levels that are up to three times normal.
- Urinary N-telopeptide of type I collagen, or uNTX is a marker of bone loss.
How do you know if you have low bone density?
The gold standard test to measure how dense (strong) your skeletal bones is a Dual Energy X-ray Absorptiometry (DEXA) test.
DEXA test is fast, painless, and fairly accurate with low radiation exposure.
Pitfalls and errors in DEXA scans are not uncommon. When DEXA studies are performed incorrectly, it can lead to mistakes in diagnosis and management.









Leave A Comment