Long COVID – What you must know
By Dr Sandra Cabot
Most people who have an infection with one of the viral variants that cause the disease of COVID-19 get better within a few weeks, but about 10% of people do not. New research led by researchers at Seattle’s Institute for Systems Biology identified factors that may predict which patients go on to suffer from longer-term disease. This research has shed light on some of the mysteries of long COVID where symptoms persist from 6 months to several years.

Symptoms of long COVID
The symptoms can be debilitating and can include:
- Loss of smell
- Cognitive impairment (foggy brain)
- Mood disorders
- Severe fatigue
- Shortness of breath
- Digestive problems
People with long COVID had signs of an overactive immune system that was misguided and caused excess inflammation. Some had features of low adrenal function with deficient levels of cortisol in the blood.
The 4 risk factors
Researchers found that four factors that were present or co-existent with initial diagnosis of COVID increased the risk of long COVID. These were:
- Diabetes type two which is often associated with fatty liver and excess weight.
- Some types of autoimmune disease such as lupus that had high autoantibody levels in the blood.
- The detection of the COVID virus genetic material (RNA) in the blood where it is more commonly found only in the saliva.
- Reactivation of the Epstein Barr Virus (EBV) which causes glandular fever (over 90% of people have evidence of EBV infection in the past but in most it stays inactive).
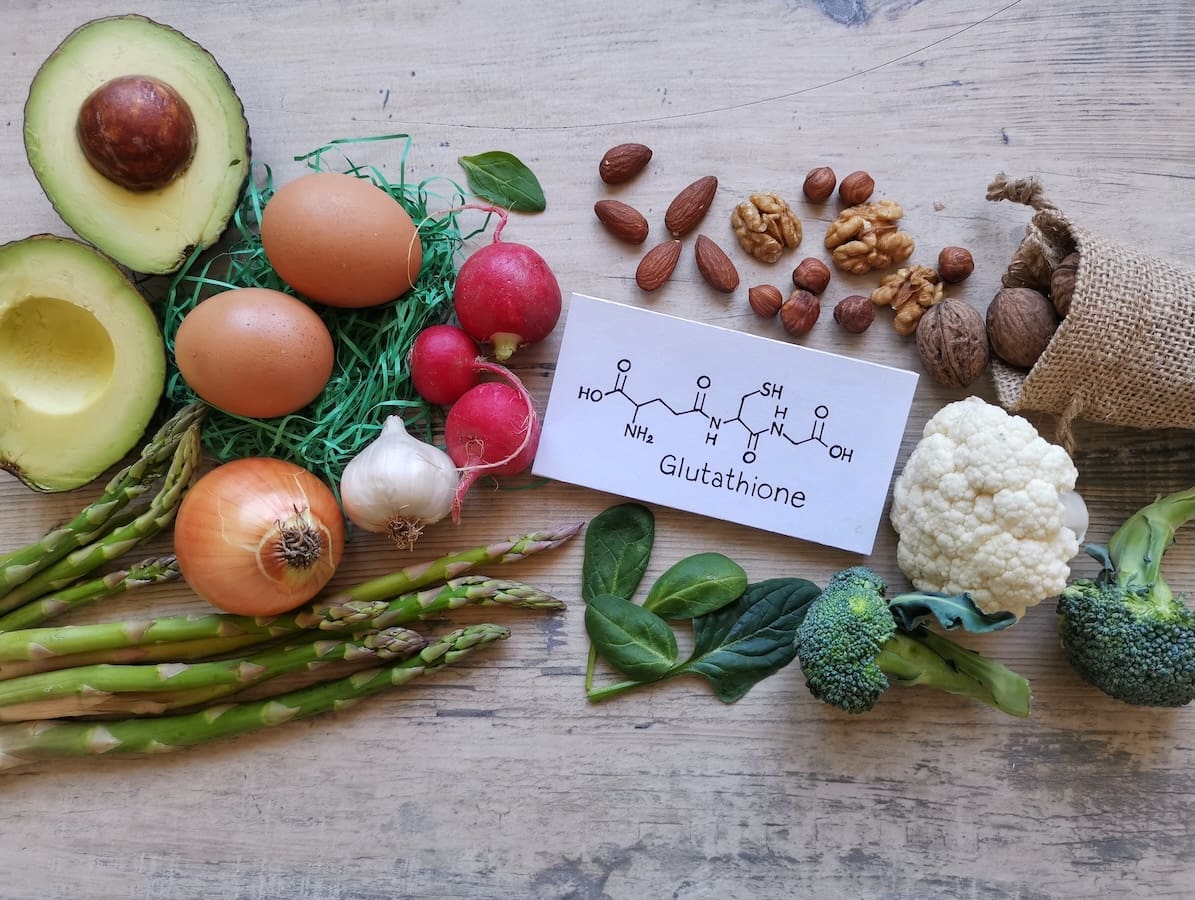
Strategies to help balance the immune system and reduce inflammation

Eat lots of veggies
Support your immune system by eating lots of vegetables. Squeezing fresh lemon or lime juice onto salads will give you vitamin C. Raw vegetable juices would be an excellent addition to your diet. Vitamin A is found in egg yolks, liver and oily fish. It helps to keep your mucous membranes healthy – your lungs, sinuses and gut lining. Zinc helps to strengthen your immune system against infections. It is found in many plant and animal foods but is easier to absorb from animal foods such as seafood and red meat.

More strategies
- Optimize your levels of vitamin D to reduce inflammation. Sunshine exposure enables your body to manufacture vitamin D. It’s best to have a blood test to ensure you have enough of this important nutrient.
- Get more sleep.
- Get more fresh air and gentle exercise to oxygenate the lungs.
- Check the function of your adrenal glands with a blood test in the early morning for cortisol levels. If low, you may need a low dose cortisone medication.
- If short of breath speak to your doctor about oxygen therapy.
If you have long COVID, we’d like to hear from you. Email us on contact@cabothealth.com.au







Am I correct in saying that vaccines are poisonous chemicals that shouldn’t be injected into anyone with auto immune condition plus COPD ?
Hi Frances,
Vaccines are a potential trigger of autoimmune disease in genetically susceptible individuals. A great deal of research has been conducted on this topic, primarily by professor Yehuda Shoenfeld.
Kind regards,
Margaret Jasinska